The CONSTANT BATTLE WITH BACTERIA
We come into the world without teeth. Too often we exit in the same condition.
That’s an odd outcome, given that enamel, the white part of the tooth, is the hardest substance in the body. Human teeth are actually as hard as sharks’ teeth, a group of scientists from Germany discovered. Sharks have advantages over us, though. Rows of sharks’ teeth are replaced throughout life, while loss of a permanent human tooth requires a prosthesis in the form of a bridge, crown, implant or dentures.
If our teeth are so strong, why then are 19 percent of the population 65 years old and older completely edentulous, or toothless?
Sharks again provide part of the answer. They don’t get cavities — and with good reason. Sharks don’t eat sugar, but we do, and apparently, plenty of it. Added sugar, such as table sugar, honey and high fructose corn syrup, are the major culprits here, but all sugars and starches play a role. The World Health Organization recommends no more than 25 grams of added sugar a day, which amounts to 20 pounds a year. Yet, the average American consumes 82 grams a day, or 66 pounds a year.
Plaque — step one to cavities
The teeth are covered by plaque a soft, invisible sticky film teeming with bacteria – some good, some bad. Plaque is always in the mouth even after you brush. That’s because bacteria are hardy creatures and multiply very rapidly. The problem begins when you start to eat. When you eat sugars or any carbohydrate or starch, like rice and bread, the bad bacteria start eating too. They feed off sugars, and that combination of sugar and bacteria is not a good thing. It produces an acid which starts the destructive process of tooth decay called caries or cavities.
The problem is that plaque will not remain soft and sticky. If not brushed away after a period of time, it turns into a hard yellowish substance called tartar, which can be removed only by a dentist or dental hygienist.
Dental caries is very common in this country. Approximately 91 percent of U.S. adults aged 20 to 64 had dental caries in permanent teeth, according to a 2015 data brief by the National Center for Health Statistics. Apparently, this process starts at an early stage. More than 43 percent of youth between the ages of two and 19 had both treated and untreated cavities in primary or permanent teeth.
Minorities are hardest hit. Blacks, Hispanics and Native Americans have the poorest oral health of any racial and ethnic groups in the United States. In addition, less educated adults experience untreated tooth decay nearly three times that of adults with at least some college education
Gum disease
Plaque is not confined to the teeth. It can also initiate an infection of your gum tissue and bone surrounding your teeth. The initial stage of gum disease is called gingivitis, which is characterized by redness and bleeding gums particularly when brushing or flossing. With good oral care, this stage is reversible. It can progress, however, to periodontitis, which is irreversible and can result in permanent tooth loss.
What’s worse is that the inflammation can have an impact on chronic diseases, such as diabetes and heart disease. “The mouth is part of the body,” said Dr. Susana Tejada, a dentist at The Dimock Center. “Bacteria that affect the mouth can travel to the rest of the body. It’s all connected.”
Research has found that plaque builds up in people with diabetes that is poorly controlled. “People with diabetes are three to four times more likely to have gum disease,” she explained. The reverse is also true. Gum inflammation makes it harder to control diabetes.
It’s not just diabetes that’s affected by poor oral health. The heart may suffer as well. Some studies suggest that clogged arteries that contribute to heart disease and stroke may have a connection to gum inflammation, according to the Mayo Clinic. Women with periodontitis have a higher risk of premature birth and low birth weight.
Dry mouth
Saliva — known more familiarly as spit — does not have the best reputation. Your mother taught you not to spit. Several states — including Massachusetts — have laws on the books forbidding residents to spit on a public sidewalk. In the Commonwealth, that antiquated law carries a whopping $20 fine. These laws and your mother’s admonition give the impression that there’s something sinister about spit. Yet, saliva is nourishing to the mouth. “It washes away food particles and moistens the mouth,” explained Tejada. “It prevents tooth decay by neutralizing the acids produced by bacteria.”
Low production of saliva results in a condition known as dry mouth. Patients complain that it feels like “cotton balls in the mouth,” or “everything seems to stick.” Dry mouth is often a side effect of certain medications, such as those to treat depression, high blood pressure, and mental health disorders anxiety and pain. Even over-the-counter drugs, including antihistamines and decongestants can cause the condition. It is more common in older people, but more probably a factor of increased use of medication than passing years. Therapy for head and neck cancers, tobacco, alcohol and marijuana use are other possible causes.
Types of dentists | |
| General dentist General dentists are your primary dental providers who manage your overall dental health. They provide cleanings and x-rays, diagnose dental conditions and perform several dental procedures, including fillings and extractions. At times, however, a specialist is required. | |
| Endodontist | specializes in root canals |
| Oral surgeon | performs complex extractions and surgeries on the mouth and jaw |
| Orthodontist | develops braces or other devices to straighten teeth |
| Pedodontist or pediatric dentist | specializes in the prevention, diagnosis and treatment of diseases that affect the gums, such as gingivitis and periodontitis |
| Prosthodontist | responsible for replacement of missing teeth and the repair of a person’s natural teeth by means of bridges, crowns, implants and dentures |
Dry mouth is more than just annoying. A more serious complication is its link to increased plaque and tooth decay. There’s no moisture to wash away the food, and therefore no protection of the teeth from acid formation. Roughly 30 percent of all tooth decay in older adults is caused by dry mouth, according to the Oral Cancer Foundation.
Over-the-counter remedies such as mouth sprays and sugar-free gum, are available to reduce the symptoms. Tejada offers an easier and free solution. “Drink a lot of water” she advised. “Sip it frequently throughout the day.”
Prevention
Yet, tooth decay and gum disease are largely preventable. You need a toothbrush, floss and fluoride toothpaste … and you have to use them. It’s easy on the budget. All together that can set you back roughly $10 every three months. Check-ups with the dentist can help spot a problem before it balloons into a more serious condition. In spite of this relatively low cost at-home treatment, cavities remain one of the most common chronic diseases in the U.S.
More than 70 percent of the residents in Massachusetts receive fluoridated water. Studies have shown that people who drink fluoridated water have a lower incidence of tooth decay. Fluoride replaces minerals in the teeth that are lost due to acid formation by bacteria.
We can drink the water, but it is necessary to do more than just imbibe and brush. Other habits do their fair share of damage. Smoking decreases the production of saliva, which leads to dry mouth, and in turn the risk of gum disease. But it’s the diet that causes the most problems, and two of the biggest offenders are soda and coffee. Roughly half of the U.S population drinks an average of three glasses of sodas every day. In addition, the average coffee drinker sips two to three cups a day, but coffee is very acidic. That means we are constantly coating our teeth with both sugar and acid, an ill-fated duo.
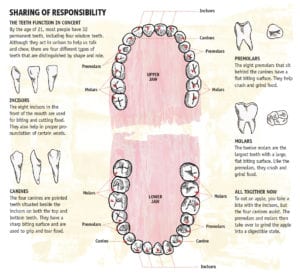
By age 21 we have 32 teeth. At 81 we should still have 32 teeth. Although, due to evolutionary changes, many people never develop their 3rd molars (wisdom teeth) or their jaws are too small to accommodate them and they are extracted, making the total tooth count 28 teeth. Tooth loss is not inevitable with age, warned Tejada. “They do not have to go hand in hand.”
Article from The Bay State Banner; Be Healthy by Karen Miller 7-20-18